New Global Guidance on CGMs During Pregnancy

If you are pregnant and living with type 1 diabetes, you are likely carrying more mental load than ever. Targets feel tighter, advice can feel inconsistent, and every glucose swing can come with an emotional reaction. Many pregnant CGM users tell us they are not sure whether they are doing enough, checking too often, or interpreting their data correctly.
In late 2025, that uncertainty eased for many people. New global guidance from the World Health Organization now clearly supports CGM for type 1 diabetes during pregnancy as part of standard, evidence based care. This is not just a clinical update. It is a signal that continuous glucose monitoring is recognised globally as a meaningful support tool during pregnancy.
This article explains what the new guidance says, why it matters for you, and how CGM for type 1 diabetes during pregnancy fits into real life care without adding pressure or fear.
What the WHO global guidance says about diabetes in pregnancy
On World Diabetes Day 2025, the World Health Organization released its first dedicated global guidelines on diabetes during pregnancy. These guidelines cover pre existing type 1 diabetes, type 2 diabetes, and gestational diabetes, with a strong focus on equitable access to care.
The WHO guidance highlights several core principles that directly support CGM for type 1 diabetes during pregnancy:
- Regular and reliable glucose monitoring throughout pregnancy
- Individualised glucose targets based on pregnancy stage
- Integration of glucose monitoring into routine antenatal care
- Improved access to essential diabetes technologies
- Multidisciplinary support rather than isolated self management
Importantly, the WHO frames glucose monitoring as a support mechanism, not a test of perfection. This approach recognises the complexity of pregnancy and the need for tools that reduce uncertainty rather than increase stress.
You can read the full WHO announcement on global guidelines for diabetes during pregnancy directly from the World Health Organization.
How this aligns with current research evidence
The WHO guidance does not stand alone. It reflects a growing body of research showing that CGM for type 1 diabetes during pregnancy improves glucose management and supports healthier outcomes.
A 2025 review published in The Lancet Global Health highlights that continuous glucose monitoring improves time in range and reduces both hyperglycaemia and hypoglycaemia during pregnancy, particularly for people with type 1 diabetes. The review also notes improved neonatal outcomes when CGM data is used consistently as part of antenatal care.
You can explore this evidence directly via The Lancet at The Lancet Global Health review on diabetes in pregnancy.

Together, these sources reinforce that CGM for type 1 diabetes during pregnancy is no longer emerging practice. It is now supported by both global policy and high quality clinical evidence.
Why CGM for type 1 diabetes during pregnancy matters
Pregnancy introduces rapid and often unpredictable changes in insulin sensitivity. Hormonal shifts can alter glucose patterns week to week and sometimes day to day.
Using CGM for type 1 diabetes during pregnancy allows you and your care team to:
- Detect rising insulin resistance earlier
- Adjust basal and bolus insulin more safely
- Reduce reliance on finger prick testing alone
- Identify overnight and post meal trends
- Make informed changes without reacting to single readings
Many people report that CGM reduces guesswork and builds confidence, especially during later trimesters when patterns change quickly.
If you are early in your CGM journey, you may find reassurance in your first Freestyle Libre sensor what to expect or do you really need a patch for your CGM.
How pregnancy CGM targets differ from everyday targets
Pregnancy targets are usually narrower than non pregnancy targets. The aim is stability and trend improvement, not constant correction.
Typical pregnancy CGM focus areas
|
CGM focus area |
How pregnancy care approaches it |
|
Target range |
Narrower and pregnancy specific |
|
Time in range |
Gradual improvement over time |
|
Overnight glucose |
Closely monitored for safety |
|
Post meal rises |
Focus on duration and recovery |
Your diabetes team may individualise these targets depending on trimester and overall health. CGM for type 1 diabetes during pregnancy supports collaboration rather than reactive decision making.
Access and equity still affect pregnant CGM users
While global guidance now supports CGM for type 1 diabetes during pregnancy, access remains uneven in some regions. Funding rules and local policies do not always keep pace with evidence.
If access has been challenging, understanding that CGM is globally recommended can strengthen advocacy conversations. You may find it helpful to explore why some people still struggle to access CGMs in the UK.
This guidance confirms that your need for CGM during pregnancy is valid, evidence based, and recognised internationally.
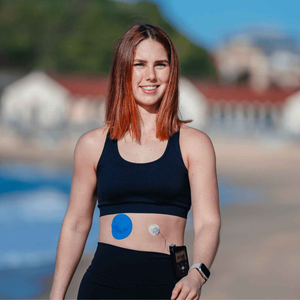
The practical side of wearing a CGM during pregnancy
Physical changes during pregnancy can affect sensor comfort and wear. Skin sensitivity, sweating, and changes in sleep position are common.
Many pregnant users find that extra support helps sensors stay secure as their body changes. Practical options such as CGM adhesive patches or skin adhesive wipes can support wear time without adding pressure.
If you have experienced lifting or irritation before, guidance on how to prep your skin for patches or how long a CGM patch should last can help you plan ahead.
Emotional wellbeing and CGM use during pregnancy
One of the most important shifts in recent guidance is the tone. CGM for type 1 diabetes during pregnancy is not presented as a tool for control or judgement.
Instead, CGM can:
- Reduce anxiety around overnight lows
- Provide reassurance between appointments
- Help partners and carers understand patterns
- Support shared responsibility rather than self blame
If pregnancy feels emotionally heavy, you may relate to when managing your diabetes becomes exhausting and how tech habits ease it.
What this guidance means for you
The message from global health bodies is clear. CGM for type 1 diabetes during pregnancy is no longer framed as optional or extra. It is recognised as a supportive, evidence based part of care.
You are not expected to manage pregnancy perfectly. You are expected to be supported with tools that reduce uncertainty and help you make informed decisions.

Whether you are pregnant, planning, or supporting someone else, this guidance reinforces what many CGM users already know. Better information builds confidence, and confidence matters during pregnancy.
References
World Health Organization 2025, WHO launches global guidelines on diabetes during pregnancy, WHO, viewed January 2026,
The Lancet Global Health 2025, Global evidence on diabetes management during pregnancy, The Lancet, viewed January 2026,
https://www.thelancet.com/journals/lanogw/article/PIIS3050-5038(25)00218-3/fulltext
Murphy, HR et al. 2020, Effectiveness of continuous glucose monitoring in pregnant women with type 1 diabetes, BMJ, viewed January 2026,
https://www.bmj.com/content/371/bmj.m3517
American Diabetes Association 2024, Standards of care in diabetes pregnancy, ADA, viewed January 2026,