When diabetes tech first enters your life, it often feels like relief. Fewer finger pricks. More clarity. A sense that things might finally be easier to manage.
But for many long-term CGM users, that feeling does not always last.
Over time, the alerts keep coming. The graphs keep updating. And the quiet expectation that you should always be responding, correcting, and improving starts to wear you down. Not suddenly. Slowly.
If this sounds familiar, you are not imagining it. You may be experiencing diabetes tech burnout.
What diabetes tech burnout looks like in real life
Diabetes tech burnout rarely shows up as outright rejection of your CGM. Most people still rely on their devices. The exhaustion is more subtle than that.
It can look like:
- feeling tense when you hear an alert, even before you check it
- letting notifications sit because you cannot deal with another decision
- feeling annoyed with yourself when glucose shifts despite doing everything right
- resenting a device you once felt grateful for.
Research into long-term technology use shows that constant exposure to glucose data can increase emotional strain and self-criticism, even when overall management improves (Barnard et al., 2024).
This kind of burnout is not about motivation or discipline. It is about mental load.
When constant data starts to feel personal
CGMs give you information in real time. That is their strength. But without space to step back, data can start to feel like judgement.
Some users describe feeling as though their numbers reflect effort or failure, even when they know logically that glucose is affected by far more than behaviour. Studies on diabetes distress support this experience, showing that continuous feedback can heighten anxiety and self-blame rather than reduce it (Powers et al., 2023).
Instead of reassurance, you might notice:
- Overthinking trend arrows
- Worry about what your clinician will think
- A sense of being watched by your own device
This emotional pressure sits at the centre of diabetes tech burnout. The technology is neutral, but the experience is not.
If this resonates, you may recognise similar patterns discussed in when managing your diabetes becomes exhausting and how tech habits ease it.
Diabetes tech burnout is not the same as diabetes distress
These two experiences are often lumped together, but they are not identical.
|
Experience |
Where it comes from |
How it feels |
|
Diabetes distress |
Living with diabetes itself |
Emotional fatigue, worry, frustration |
|
Diabetes tech burnout |
Constant interaction with devices |
Alert fatigue, avoidance, resentment |
You can feel grateful for your CGM and still feel worn down by it. That distinction matters, because it changes what support actually helps.
Recognising diabetes tech burnout allows you to adjust how technology fits into your life, rather than feeling like the answer is to try harder.
Alerts are helpful - until they are not
Alerts save lives. That part is not up for debate. But they are also one of the most common sources of fatigue for long-term users.
Research shows that frequent alerts can increase stress and disengagement, particularly when people feel they cannot respond perfectly every time (Wang et al., 2022). Over time, this can lead to alert avoidance rather than better outcomes.

If alerts are draining you, it may help to:
- Revisit thresholds with your care team
- Reduce non-essential notifications
- Allow yourself quieter periods when it is safe to do so
Many people navigate this balance daily, as explored in how CGM alerts affect workdays and how people manage them.
Choosing fewer alerts is not giving up. It is choosing sustainability.
Wearing diabetes tech all the time has a cost
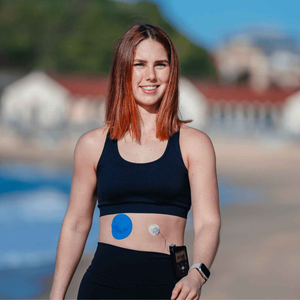
Burnout is not only emotional. There is also the physical reality of wearing devices continuously.
Over months and years, some people notice:
- fatigue from always having something attached
- resistance to changing sensors
- frustration when patches fail or irritate skin.
These small annoyances add up. Research shows that physical discomfort and device burden contribute to emotional exhaustion, especially for experienced users (Barnard et al., 2024).
Reducing friction where you can matters. Practical steps like improving skin prep, explored in how to prep your skin for patches the right way to make them last, can remove one source of daily stress.
Some people also find that supportive options like patches from the Type Strong CGM patches collection reduce constant worry about sensors shifting or failing, without changing how they engage with data.
What the research actually tells us
The evidence is clear on one thing. Diabetes technology improves access to information. What it does not guarantee is emotional relief.
Reviews of diabetes tech use consistently show that psychological outcomes depend on how technology fits into daily life, not just on accuracy or frequency of data (Barnard et al., 2024). Emotional wellbeing improves when people feel autonomy, flexibility, and permission to adapt tools to their needs.

Another consistent finding is timing. Diabetes tech burnout often appears after the early phase of enthusiasm, when the expectation becomes “I should have this under control by now” (Wang et al., 2022).
That expectation is heavy. And unrealistic.
People also ask
Does diabetes technology cause burnout?
For some people, yes. While diabetes technology can reduce workload, it can also increase emotional pressure when alerts, data, and expectations feel constant (Wang et al., 2022).
How do people manage diabetes tech burnout?
Most people manage diabetes tech burnout by adjusting alerts, setting boundaries with data, reducing physical discomfort, and reframing glucose information as feedback rather than judgement (Powers et al., 2023).
Is it normal to feel overwhelmed by CGM data?
Very normal. Research shows that long-term CGM users often experience data fatigue, even when their overall management is stable (Barnard et al., 2024).
Should you take a break from diabetes technology?
Some people benefit from planned breaks or reduced engagement, but changes should always be made safely and discussed with a healthcare professional (Everyday Health, 2024).
Finding a way to live with tech, not under it
Diabetes tech is meant to support you, not measure your worth. Feeling tired of it does not mean you are doing something wrong. It means you have been carrying a lot.
Diabetes tech burnout is real, increasingly recognised, and more common than many people admit. You are allowed to shape how technology fits into your life. You are allowed to protect emotional energy. And you are allowed to need support, even if you have been doing this for years.
At Type Strong, we believe the goal is not perfect data. It is sustainable living. When technology works quietly in the background, it leaves more room for confidence, rest, and trust in yourself.
References
Barnard, K., Crabtree, V., Adolfsson, P. and Heller, S., 2024.
Psychological impacts of diabetes technology use. Diabetes Therapy, 15(3), pp. 1–12.
Powers, M.A., Bardsley, J., Cypress, M. and Funnell, M.M., 2023.
Diabetes distress and diabetes technology. Practical Diabetes, 40(2), pp. 45–51.
Wang, Y., Lim, A. and Smith, J., 2022.
Digital health technologies and diabetes-related distress - balancing benefits and burden. Diabetes Research and Clinical Practice, 186, 109118.
Everyday Health, 2024. How to beat diabetes tech distress. Everyday Health.