It might feel like you’re already juggling enough – medications, monitoring, diet, and appointments – but here’s one more essential habit worth scheduling: your next eye screening.
A 2025 study by University College London found that adults with diabetes and persistently high glucose levels were three times more likely to develop diabetic eye disease than those with well-controlled levels (University College London, 2025).
That’s a powerful reminder for anyone living with type 1 or type 2 diabetes long term. Even if your vision feels fine now, diabetic retinopathy often develops silently. This article breaks down why glucose control matters so much, how often to screen, what to expect from your check-up, and how to align your CGM routine with protecting your eyes.
Why high glucose levels raise diabetic eye-disease risk
The University College London study followed over 7 000 participants for 14 years and found:
- Those with uncontrolled diabetes had a 31 % chance of developing diabetic eye disease.
- Those with controlled levels had about a 9 % chance.
- Participants with consistently high glucose were also more prone to glaucoma and macular degeneration (University College London, 2025).
These findings align with other public-health data showing that chronic hyperglycaemia damages the retinal capillaries – the fine blood vessels at the back of the eye – causing leakage, swelling, and eventual vision loss (Diabetes UK, 2024).
Good glucose management doesn’t just protect your A1c numbers – it protects your vision.
Who should prioritise an eye screening now
Certain people face higher risk for diabetic retinopathy. You should book a screening as soon as possible if you:
- Have had type 1 diabetes for more than 5 years or type 2 diabetes for over 10 years
- Often record HbA1c readings above your target
- Also have high blood pressure or cholesterol
- Smoke or have cardiovascular issues
- Have missed previous screening invitations

People also ask
How often should someone with diabetes have an eye exam?
According to Australian and UK screening programmes, most adults with diabetes should have a dilated retinal exam every 12 months (RANZCO, 2022; NHS England, 2023).
If no retinopathy is found and you’re considered low risk, your optometrist may extend this to every 24 months – but annual checks remain the safest choice.
What happens during diabetic eye screening?
A standard screening includes:
- Visual acuity testing – reading letters on a chart
- Pupil dilation with safe eye drops
- Retinal photography or fundus imaging to capture the back of your eye
- OCT scanning in some clinics to assess for macular swelling
The entire visit takes around 20–30 minutes. After dilation, your sight may blur temporarily, so plan alternative transport (Macular Disease Foundation Australia, 2024).
Can diabetic eye disease be prevented?
Complete prevention isn’t always possible, but progression can often be slowed or stopped through:
- Tight blood-glucose management
- Stable blood pressure and cholesterol
- Quitting smoking
- Regular screening and early treatment
Laser therapy and anti-VEGF injections are highly effective when eye disease is detected early (Macular Disease Foundation Australia, 2024).
What symptoms require urgent attention?
Seek immediate review if you notice:
- Sudden floaters or flashing lights
- Blurred or distorted central vision
- Dark patches or shadows in your sight
These may indicate bleeding or retinal detachment, both requiring prompt care (NHS England, 2023).

Recommended diabetic eye-screening schedule
|
Clinical situation |
Interval |
Notes |
|
No retinopathy, low risk |
Every 12 months |
Some low-risk patients may extend to 24 months |
|
Mild non-proliferative retinopathy |
Every 12 months |
Maintain glucose and BP control |
|
Moderate–severe retinopathy |
Every 3–6 months |
Ophthalmology supervision recommended |
|
After treatment (laser/injection) |
As advised |
Often every 3–4 months |
Adapted from RANZCO (2022) Screening and Referral Pathway for Diabetic Retinopathy.
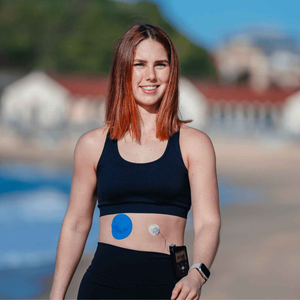
How CGM users can protect their eyes daily
1. Use your CGM as a prevention tool
Your continuous glucose monitor (CGM) helps identify sustained highs before they silently affect your blood vessels.
If you use adhesive patches, focus on proper skin preparation to avoid irritation. See our guide on proper skin prep and tips for extra protection in summer.
Using hypoallergenic CGM patches can also improve comfort and consistency, helping you stay connected to your readings without interruption.
2. Keep blood pressure and cholesterol under control
Hypertension and lipid imbalance amplify retinal-vessel stress. Work with your GP to manage both alongside your diabetes plan.
3. Avoid smoking and protect vascular health
Smoking restricts oxygen flow to the retina and worsens glycaemic control. Quitting reduces your retinopathy risk dramatically (Macular Disease Foundation Australia, 2024).
4. Set reminders for annual checks
Register with Australia’s KeepSight program or your country’s national reminder service to get automatic recall notifications (Macular Disease Foundation Australia, 2024). Mark your own calendar too – consistency saves sight.
After your screening: understanding your results
Screening results are typically categorised as:
- No retinopathy – continue routine checks
- Background/mild changes – maintain annual visits
- Referable retinopathy – ophthalmologist follow-up required
Always inform your GP and diabetes care team so results guide your ongoing management (NHS England, 2023). For CGM users, maintaining stable glucose trends can reduce further vascular damage – see our guide on how long a CGM patch should last for tips on reliable wear.
Build vision protection into your daily routine
Vision care and glucose monitoring go hand in hand. By combining consistent CGM tracking with healthy skin practices and annual screenings, you strengthen your defence against vision loss.
If you’re active, travel often, or attend frequent appointments, Type Strong’s Dexcom G7 patches and Medtronic Guardian patches are designed to stay secure and gentle on skin. For multi-sensor users, the CGM patch bundle helps you stock up while saving.
References
Diabetes UK (2024) Eye health and diabetes. Available at: https://diabetes.org/health-wellness/eye-health (Accessed 14 October 2025).
Macular Disease Foundation Australia (2024) Diagnosing and reducing risk of diabetic eye disease. Available at: https://www.mdfoundation.com.au (Accessed 14 October 2025).
NHS England (2023) Your guide to diabetic eye screening. Available at: https://www.gov.uk/government/publications/diabetic-eye-screening-description-in-brief (Accessed 14 October 2025).
RANZCO (Royal Australian and New Zealand College of Ophthalmologists) (2022) Screening and Referral Pathway for Diabetic Retinopathy. Available at: https://ranzco.edu (Accessed 14 October 2025).
University College London (2025) High glucose levels in people with diabetes linked to tripling of eye-disease risk. Available at: https://www.ucl.ac.uk/news/2025/jul/high-glucose-levels-people-diabetes-linked-tripling-eye-disease-risk (Accessed 14 October 2025).