January arrives with a familiar message; reset, restart, be better. For many people living with a CGM, this pressure can feel amplified. You may look at your CGM data after the holidays and feel an urge to fix everything at once - tighter food rules, harder exercise, fewer glucose rises, cleaner graphs.
Yet many CGM users find that January health resets do not lead to motivation. Instead, they lead to frustration, stress, and burnout. If this sounds familiar, it is not because you lack discipline. It is because January resets often ignore how CGMs, bodies, and emotions actually work together.
This article explains why the CGM January reset often backfires, what your data is really reflecting at this time of year, and how to approach motivation in a way that supports both glucose stability and mental wellbeing.
Why the CGM January reset feels so appealing
After December, CGM users often notice higher averages, more variability, or disrupted routines. Because CGM data is constant and visible, it can feel urgent and personal.
A typical CGM January reset promises:
- Control after holiday disruption
- Motivation through strict goals
- The belief that better CGM numbers equal better health
However, CGM data is not a judgement of effort. It reflects hormones, stress, sleep, illness, temperature, activity levels, and recovery. When January resets treat CGM data as a scorecard, they set unrealistic expectations from the start.
How winter physiology affects CGM users
January is not a neutral month for glucose. Seasonal and environmental factors influence insulin sensitivity and glucose variability, particularly for people with type 1 diabetes.
Common winter influences on CGM readings (Northern Hemisphere)
- Reduced insulin sensitivity in colder temperatures
- Shorter daylight hours affecting sleep quality
- Increased illness and immune response
- Lower overall movement compared to warmer months
Research shows that seasonal changes can affect glycaemic control, independent of behaviour (Tseng et al., 2005). If your CGM looks different in January, it is likely reflecting biology, not failure. For a deeper explanation, see how changing seasons affect blood sugar.
How summer physiology affects CGM users
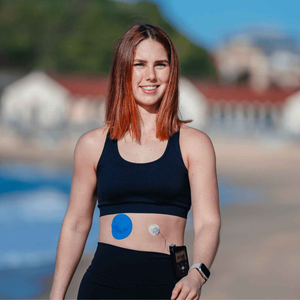
For many CGM users in Australia and across the Southern Hemisphere, January is not about winter routines. It is peak summer. Heat, humidity, holidays, and changes in daily structure can all influence how your glucose behaves and how your CGM data appears.
If your CGM readings feel less predictable during summer, this is a normal physiological response rather than a sign that your management is slipping.

Common summer factors that influence CGM data (Southern Hemisphere)
During warmer months, CGM users may experience:
- Increased insulin sensitivity due to heat-related vasodilation
- Faster insulin absorption, particularly during movement or exercise
- Greater glucose variability linked to dehydration
- Less consistent meal timing during holidays and travel
- Increased sweating, which can affect sensor adhesion and wear time
Heat exposure and dehydration can alter interstitial fluid balance, which CGMs rely on to estimate glucose levels. This can result in quicker rises or drops that are not always directly related to food intake (Adams et al., 2015).
Why summer CGM patterns can feel harder to control
Summer often brings more spontaneous activity, later nights, social eating, and travel. When a resolution-driven January reset is layered on top of these seasonal changes, it can feel overwhelming.
For CGM users in summer climates, rigid targets and strict rules may increase stress rather than improve glucose stability. This is one reason January health resets often backfire for Southern Hemisphere users in particular.
For more context on hydration and glucose trends, see dehydration and diabetes.
Summer heat, skin, and CGM wear
Summer also introduces practical challenges that can affect motivation. Sweat, sunscreen, salt water, and frequent showers can reduce patch adhesion. When a sensor loosens early, it can interrupt CGM data and add unnecessary frustration.
You may find these resources helpful:
Supporting consistent CGM wear during summer can help reduce friction and make it easier to stay engaged without adding pressure.
A seasonal mindset shift for Southern Hemisphere CGM users
If you are experiencing summer rather than winter, it may help to reframe January as a maintenance phase rather than a reset. Many CGM users find summer management more sustainable when it prioritises:
- Hydration over restriction
- Trend awareness over daily perfection
- Flexibility during holidays and social events
- Reliable CGM wear to reduce avoidable disruptions
Your CGM is still providing valuable insight, even when the graphs look messier. Interpreting your data through a seasonal lens allows you to work with your body rather than against it.
When motivation turns into pressure for CGM users
Motivation can be helpful, but resolution-driven behaviour often becomes rigid when paired with constant CGM feedback.
Signs your CGM January reset may be backfiring include:
- Checking your CGM more often but feeling more anxious
- Feeling discouraged by normal glucose rises
- Avoiding foods rather than learning from patterns
- Feeling disappointed despite sustained effort
Psychological stress increases cortisol levels, which can raise glucose levels and increase variability (Hackett and Steptoe, 2017). Pressure can work against the outcomes you are trying to improve.
The mismatch between reset culture and CGM reality
January resets often rely on all-or-nothing thinking. CGMs work best when used for long-term pattern recognition.
|
Reset thinking |
CGM reality |
|
Perfect days matter |
Trends over time matter |
|
Glucose rises are bad |
Rises provide useful feedback |
|
Strict rules create success |
Sustainability creates success |
|
One bad day undoes progress |
Glucose adapts daily |
When expectations do not match how CGMs function, frustration is almost inevitable.
Why CGM burnout is common in January
January follows a demanding period of self-management, social pressure, and disrupted routines. Many CGM users start the year already fatigued.
Burnout is linked to reduced self-care, increased distress, and poorer glycaemic outcomes (Fisher et al., 2014). Pushing harder during this period can deepen disengagement rather than restore motivation.
You may find reassurance in this discussion on diabetes burnout.

A more supportive alternative to the CGM January reset
Instead of resetting everything, many CGM users benefit from recalibration.
What recalibration looks like
- Focusing on one small, achievable change
- Observing CGM patterns without judgement
- Using data to guide curiosity, not punishment
- Reducing friction from practical issues like sensor wear
Reliable sensor wear matters. Patch failure or irritation adds unnecessary stress. Supportive CGM patches can help reduce interruptions so your focus stays on learning from your data.
January comfort, skin, and CGM consistency
Seasonal skin changes can affect CGM adhesion. Dry skin in winter or moisture in summer can both shorten wear time.
Helpful guides include:
Small adjustments can improve consistency without increasing pressure.
People Also Ask
Why are my CGM readings worse in January?
Seasonal physiology, stress, illness, hydration, and routine changes can all affect glucose levels. This is common and not a personal failure.
Should I reset my diet based on CGM data?
Gradual adjustments are generally more sustainable. CGM data works best when used to test small changes over time.
Can stress affect CGM readings?
Yes. Stress hormones such as cortisol can raise glucose levels and increase variability.
How can I stay motivated with a CGM without burning out?
Focus on trends rather than perfection, and allow flexibility. Motivation lasts longer when paired with self-compassion.
Moving forward without the reset mindset
If January feels heavy, it does not mean you are managing diabetes wrong. It means you are navigating a demanding season with a complex condition. CGMs are powerful tools, but they work best with realistic expectations and emotional support.
You do not need a reset to move forward. Small, steady adjustments - supported by reliable CGM wear and a compassionate mindset - often lead to better outcomes than any January overhaul ever could.
References
Fisher, L., Hessler, D.M., Polonsky, W.H. and Mullan, J. (2014) ‘When is diabetes distress clinically meaningful? Establishing cut points for the Diabetes Distress Scale’, Diabetes Care, 37(3), pp. 673–680. Available at: https://diabetesjournals.org/care/article/37/3/673/37754 (Accessed: 14 January 2026).
Hackett, R.A. and Steptoe, A. (2017) ‘Type 2 diabetes mellitus and psychological stress - a modifiable risk factor’, Current Diabetes Reports, 17(3), pp. 1–9. Available at: https://link.springer.com/article/10.1007/s11892-017-0844-3 (Accessed: 14 January 2026).
Tseng, C.L. et al. (2005) ‘Seasonal patterns in glycaemic control in patients with diabetes mellitus’, American Journal of Managed Care, 11(6), pp. 407–412. Available at: https://www.ajmc.com/view/june05-2091p407-412 (Accessed: 14 January 2026).