For many people living with diabetes in the UK, continuous glucose monitors (CGMs) are no longer seen as emerging technology. They are widely recognised as tools that improve safety, confidence, and day-to-day glucose awareness. Yet, access remains uneven. If you have ever been told you are eligible but still cannot get a sensor, or you are managing your device without reliable dexcom patches, you are not alone.
This article explores why access gaps persist, what this means for health equity, and how UK CGM users and advocates can navigate the system more effectively.
CGMs in the UK – policy versus lived experience
National Institute for Health and Care Excellence (NICE) guidance has expanded CGM eligibility in recent years. Real-time CGMs are now recommended for most people with type 1 diabetes and some people with insulin-treated type 2 diabetes.
However, implementation is inconsistent. Local Integrated Care Boards (ICBs) interpret guidance differently, leading to postcode variation. This affects not only sensors themselves but also access to practical support tools such as dexcom patches, which are rarely included despite being essential for keeping sensors functional.
Why access still varies across the UK
Local commissioning decisions
Funding decisions are made locally, meaning two people with identical clinical needs may receive different outcomes depending on where they live.
Workforce and service pressure
Under-resourced diabetes teams may delay CGM rollout due to training demands, staffing shortages, or administrative backlogs. Adults transitioning from paediatric care are particularly affected.
Advocacy and awareness gaps
Some people are never told they qualify. Those less confident in clinical conversations may miss out entirely, reinforcing health inequity.
The hidden access issue – keeping your CGM on
Receiving a CGM is only part of the story. Adhesion failure is a leading cause of early sensor loss, and replacement is not always straightforward. When this happens, users are often left to self-fund protective supplies.
This is where dexcom patches uk play a practical role. Overpatches can reduce sensor loss, minimise skin irritation, and support full wear time. The importance of protection is explained in why your CGM sensor needs extra protection in summer.
Who is most affected by CGM access barriers?
|
Group |
Common barriers |
|
Adults with type 1 diabetes |
Local funding variability |
|
People with type 2 diabetes on insulin |
Narrow eligibility interpretation |
|
Rural UK residents |
Limited specialist access |
|
Lower-income households |
Cost of replacement supplies |
|
Minority ethnic groups |
Lower referral and advocacy rates |
These barriers often mean managing diabetes with less data than clinically recommended.

People Also Ask
Why are CGMs not available to everyone on the NHS?
Although NICE provides national guidance, local funding and service capacity determine access. This leads to inconsistent rollout.
Can you get Dexcom on the NHS in the UK?
Yes, Dexcom CGMs are available for eligible patients. However, accessories such as dexcom patches uk are often not routinely supplied.
Why do some GP practices not offer CGMs?
GPs usually follow guidance from specialist diabetes teams. Limited training or unclear funding pathways can delay availability.
Do you have to pay for CGM patches in the UK?
Often, yes. While sensors may be funded, many users self-source dexcom patches uk to reduce early sensor loss.
What you can do if access feels blocked
Practical steps that may help include:
- Asking your diabetes team to document clinical need clearly
- Referencing NICE NG17 guidance directly
- Keeping records of sensor loss due to adhesion issues
- Using reliable dexcom patches uk to improve wear time
- Engaging with patient advocacy organisations
For realistic expectations around wear time, see how long should a CGM patch last.
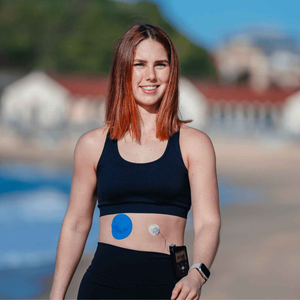
Supporting your CGM day to day
While policy reform takes time, protecting the CGM you already have is something you can control. Many UK users rely on purpose-designed overpatches to support daily movement and reduce skin stress.

Type Strong offers a range of options through its CGM patch collection, designed to support consistent wear for all cgm users.
Skin preparation also plays a role. How to prep your skin for patches explains evidence-based steps that improve adhesion.
Looking ahead – equity is about consistency, not just devices
True access means more than being handed a sensor. It means having the support to wear it confidently and continuously. When access depends on postcode, persistence, or personal finances, inequity remains.
As UK CGM users and advocates, sharing knowledge and supporting one another matters. Whether that means pushing for funded devices or choosing dependable uk dexcom patches to protect your sensor, every step helps build stability in your care.
You deserve reliable data, not unnecessary obstacles.
References
Diabetes UK (2023) Continuous glucose monitoring and flash glucose monitoring. Available at: https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/continuous-glucose-monitoring (Accessed: 14 January 2026).
National Institute for Health and Care Excellence (2022) Type 1 diabetes in adults: diagnosis and management (NG17). Available at: https://www.nice.org.uk/guidance/ng17 (Accessed: 14 January 2026).
NHS England (2023) Diabetes technology funding and access. Available at: https://www.england.nhs.uk/diabetes/diabetes-technology/ (Accessed: 14 January 2026).