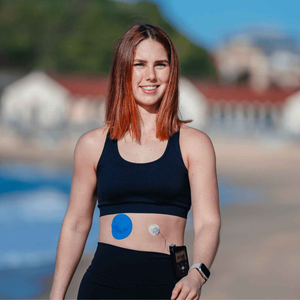
From the outside, you might look completely healthy. But what others can’t see is the device under your shirt or patch on your arm quietly working to track your blood glucose. For many people with type 1 or type 2 diabetes, this hidden tool is a continuous glucose monitor (CGM). While life-changing, it can also feel like part of an invisible illness CGM journey – a daily reality that others may never understand.
Living with an invisible illness can be both empowering and exhausting. On one hand, you have the tools to take control of your health. On the other, it can feel like the world doesn’t always recognise the invisible challenges you carry. This is why conversations about invisible disabilities matter – they give language to what so many people experience but find difficult to explain.
What is an invisible disability?
“Invisible disabilities are defined as physical, mental, or neurological conditions that are not visible from the outside, yet can limit or challenge a person’s movements, senses, or activities.” – Invisible Disabilities Association.
Diabetes often falls into this category. You may not look unwell, but your day is filled with decisions, monitoring, and adjustments that others simply don’t see. A CGM doesn’t change the fact that your condition is invisible – it just adds another layer: invisible tech working constantly in the background.
Why a CGM feels like invisible illness tech
One of the most powerful features of a CGM is its ability to blend into daily life. The sensor usually sits under clothing, with only a patch or small device visible. Yet while invisible to others, it becomes an ever-present part of your day.
For some, this invisibility is a blessing – no need to answer questions or explain your condition in every social setting. For others, it can feel isolating. Friends, colleagues, or even family may not recognise the effort involved in living with diabetes because they can’t see it.
This hidden aspect is why so many users describe their CGM as invisible illness tech – a quiet companion that keeps you safe while reminding you of the work you do daily.
(If you’ve ever struggled with how others perceive your device, you might relate to our reflections on wearing a CGM in public).
Challenges of invisible illness CGM users
Social misunderstandings
People often say, “But you don’t look unwell.” This can make it difficult to share your experiences without feeling like you need to justify them. On the rare occasions your sensor or patch is noticed, it can bring awkward questions or even unwanted assumptions.
Practical patch struggles
Alongside social challenges, there are practical ones. Patches can peel, edges may lift, and some people develop irritation. These issues add another layer of invisible stress to CGM wear. Knowing how to spot patch reactions can make a big difference to comfort and peace of mind.
Mental health impact
Living with an invisible disability is not just physical – it affects your mental health too. Many CGM users share that while they are proud of their proactive management, they can also feel drained by the constant responsibility. This is part of what we explored in our piece on diabetes tech and mental health.
Support tools for invisible CGM wear
One way to make living with invisible illness tech easier is to use supportive tools. CGM patches are more than just adhesive – they are confidence-builders.
- A strong patch keeps your sensor secure through movement, sweat, or sleep.
- Skin adhesive wipes can help sensors last longer and reduce edge lift.
- A varied collection of CGM patches lets you choose breathable, hypoallergenic materials designed for comfort.
When you’re managing something invisible to others, small physical supports can create big emotional relief.
Invisible challenges vs Practical support
|
Invisible CGM challenge |
How to support it |
|
Others not seeing daily effort |
Share your story, educate when you feel ready |
|
Patch irritation |
Use hypoallergenic CGM patches |
|
Fear of sensor peeling |
Adhesive wipes or tape roll |
|
Feeling isolated |
Join online and in-person diabetes communities |
People also ask
Is diabetes an invisible disability?
Yes. While not always visible, diabetes requires constant management and can affect daily activities. This makes it part of the invisible disability category.
Why is a CGM considered invisible illness tech?
Because it often sits under clothing or discreet patches, a CGM works continuously without being seen by others. It represents a hidden but vital form of support.
How can you explain your CGM to friends or colleagues?
Keep explanations simple. For example: “It’s a medical device that helps me track blood sugar in real time.” You can share more detail if you feel comfortable, but you don’t owe anyone lengthy explanations.
What support can make invisible illness easier to manage?
Community support, secure CGM patches, and open conversations about invisible disabilities can reduce the burden and help you feel less alone.
Do CGM patches help people feel more confident wearing their device?
Yes. A well-secured sensor means fewer worries about peeling or irritation, which translates to greater confidence in daily life.
Living proudly with invisible illness CGM tech
Your CGM may be invisible to others, but it is never invisible to you. It represents your strength, your care, and your ability to manage diabetes on your own terms. Being part of an invisible disability community doesn’t mean being unseen – it means being connected to millions of people who understand the quiet work you do every day.
At Type Strong, we believe your invisible tech deserves visible support. Whether that’s through reliable patches, adhesive wipes, or simply knowing you are not alone, you have every reason to live proudly with your invisible illness CGM.