Let’s talk about something we don’t talk about enough.
Mental health.
Diabetes.
And men.
This Men's Health Week, we wanted to write a dedicated blog for our male customers, living with diabetes. If you’ve ever felt like you’re supposed to “just get on with it” while managing blood sugars, work, family, and everything in between — you’re not alone. There’s long been a silence around men’s emotional wellbeing, and diabetes often makes that silence louder.
But here’s the truth: mental health and diabetes are deeply connected. And the pressure to appear strong or “in control” can sometimes make it harder for men to reach out. Thankfully, that’s starting to shift — and technology is playing a quiet but important role in making day-to-day management less overwhelming.
Why Mental Health and Diabetes Go Hand-in-Hand
Living with diabetes isn’t just about numbers or nutrition — it’s a constant mental load. You’re making decisions all day: What to eat. When to move. Whether you’re high or low. Whether it’s safe to go for a run or drive the kids to school.
That decision fatigue builds up — especially if you’re aiming for “perfect control” all the time.
In fact, research shows people with diabetes are two to three times more likely to experience depression than those without it.
"The physical symptoms of diabetes can cause mood swings, anxiety and confusion, while the stress of managing the condition sometimes results in diabetes distress." - The Australian & New Zealand Mental Health Association
Despite that, many men don’t reach out — whether it’s due to stigma, time, or simply not realising how closely connected their mental state is to their glucose trends.
The Reality of Diabetes Burnout
If you’ve ever found yourself thinking, “I just can’t be bothered today,” you’re not lazy — you might be burnt out. Diabetes burnout is real, and it’s not talked about enough, particularly among men.
It can look like:
- Avoiding blood sugar checks
- Ignoring alarms
- Skipping appointments
- Feeling resentful or guilty
- Saying “what’s the point?” more than usual
It’s the kind of fatigue that doesn’t go away with a nap. And often, people carry it in silence.
What Holds Men Back From Speaking Up?
Let’s face it — there’s still a cultural undercurrent that says men should “power through” and not complain. But mental health isn’t weakness, and managing diabetes is no small task.
Common reasons men hold back:
- Fear of being judged
- Pressure to appear capable
- Not knowing how to talk about emotions
- Prioritising work or family over personal wellbeing
The first step? Acknowledging that it’s okay not to be okay. The second? Knowing there are tools — including diabetes tech — that can ease the mental strain.

How CGM Tech Helps Ease the Load
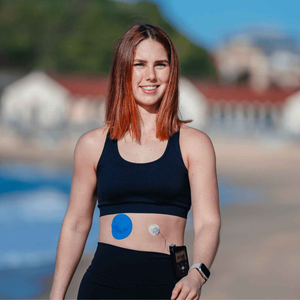
Here’s where things start to shift. Continuous Glucose Monitors (CGMs), like the Dexcom G7 or Freestyle Libre, don’t just provide numbers — they provide relief. Real-time readings, alerts, and trend arrows take some of the guesswork out of your day.
And that matters. Here’s how CGMs support emotional wellbeing:
- Less uncertainty: Real-time data helps reduce anxiety around unexpected highs and lows
- Better sleep: Night-time alerts reduce fear of hypos while sleeping
- Less pain: No finger pricks = less stress
- Data over guilt: Helps you learn patterns instead of blaming yourself
- Improved confidence: Knowing you’re staying in range more often builds momentum
Even something as simple as reducing the number of daily decisions can have a positive impact on mental health. It’s not about perfection — it’s about lightening the mental load.
Small Fixes That Make a Big Difference
But what happens when your sensor doesn’t stay put? Or worse, when it starts irritating your skin?
It may sound minor, but when your CGM falls off during the night or starts itching on day three, it becomes another point of stress. That’s where the right adhesive can change everything.
Our customer reviews often mention that finding the right patch made all the difference — giving them the confidence to move more, rest better, and focus less on whether their device would stay put.
When your gear sticks, you stick with your routine — simple as that.
And if you need more flexibility for your setup, you can always build your own patch bundle to suit whatever device you're using, no matter how often you rotate sites or switch arms.
Mental Health Tools That Don’t Look Like Therapy
Not every tool for mental health looks like a therapist’s couch. For many men, it’s about small, consistent things that offer clarity or relief.
Here are a few that genuinely help:
- Using a CGM to reduce uncertainty
- Exercising to manage mood and blood sugar
- Wearing a patch that doesn’t budge — so you're not second-guessing your sensor
- Talking to a mate, not just a doctor
- Accepting bad days without letting them spiral into bad weeks
And if the emotional load gets heavy? Speaking to a GP, diabetes educator, or psychologist can make all the difference — even just once.
Final Thoughts
Living with diabetes as a man can be a quiet battle — one that’s often invisible to the people around you. But it doesn’t have to stay that way.
Mental health and diabetes are connected every single day. And whether you find support in a CGM, in a conversation, or in a small win like finally finding a patch that doesn’t peel off — it all counts.
So let’s keep talking. Let’s keep supporting each other. And let’s make room for wellbeing — not just blood sugar levels — in the way we manage diabetes.
Need better support for your sensor or infusion set?
Our skin-safe patches are designed for Dexcom, Libre, Omnipod, Medtronic and infusion sites — so you can focus on your health, not your adhesive.