If you’ve been living with diabetes for a while, you’ll know how easy it is to focus on your numbers – the graphs, alerts, and sensor data that tell you how your body’s doing. But what many people don’t realise is that high glucose can start damaging the heart quietly, often years before any warning signs appear. You might feel perfectly fine, yet small changes could already be taking place inside your arteries.
That’s why understanding your diabetes heart disease risk matters. This isn’t about fear; it’s about insight. Knowing how sugar affects your heart and what you can do each day to protect it can make all the difference later on.
How high glucose quietly harms your heart
Heart problems linked to diabetes rarely happen overnight. They tend to creep up slowly – the result of sugar circulating in the bloodstream and irritating vessel walls. Diabetes UK explains it clearly: “High blood sugar levels can damage blood vessels and the nerves that control your heart over time.”
When glucose stays high, it attaches to proteins in the artery lining. That makes the vessels less flexible and more likely to trap cholesterol or plaque. Over time, the heart must work harder to pump blood through these narrowed channels. You might not notice much at first – maybe a little fatigue, or breathlessness on the stairs – but it’s the start of a pattern that can lead to serious trouble if left unchecked.
The good news is that this process can be slowed, and even partly reversed, when glucose levels are managed consistently.
Why people with diabetes face higher heart risks
According to the World Health Organization, adults with diabetes are two to three times more likely to develop heart disease than those without it. High glucose is only one piece of the puzzle; factors such as raised cholesterol, high blood pressure, and chronic inflammation often appear alongside it.

Your diabetes heart disease risk rises when:
- Glucose levels swing widely throughout the day
- Your CGM sensor loses adhesion, creating gaps in data
- Illness, dehydration, or stress trigger prolonged highs
Each of these pressures makes the heart work harder. The more stable your readings are, the easier it becomes for your cardiovascular system to cope.
How CGM technology helps you spot early warning patterns
Continuous Glucose Monitoring (CGM) doesn’t just keep you informed – it can show how everyday choices influence your long-term heart health. A pattern of overnight highs, for instance, could point to dietary or medication timing issues worth discussing with your care team.
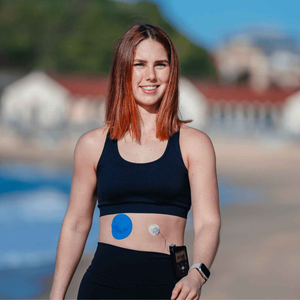
For your CGM to collect accurate data, it needs to stay in contact with the skin. A secure patch is vital. Type Strong’s CGM patches help prevent signal loss and discomfort, even through workouts or hot days. If you’ve ever struggled with edges peeling or sensors shifting, Type Strong Skin Adhesive Wipes add extra staying power and a clean surface for application.
Reliable readings mean clearer insights – and that gives you more control over the choices that protect your heart.
How glucose-related heart strain develops
|
Stage |
What happens inside the body |
What you might notice |
|
Early (often silent) |
Sugar affects artery linings and nerves |
Slight tiredness, mild dizziness after meals |
|
Progressive strain |
Blood flow decreases as arteries stiffen |
Breathlessness or chest pressure during activity |
|
Advanced stage |
Oxygen can’t reach heart muscle properly |
Persistent chest pain or irregular heartbeat |
Everyday habits that strengthen heart and glucose health
The NHS reminds people with diabetes that keeping glucose, blood pressure, and cholesterol in healthy ranges dramatically lowers heart-disease risk. The key is building simple, repeatable habits:
- Watch your patterns. Notice when your CGM readings rise or drop sharply – that’s valuable information.
- Prepare your skin well. Proper skin prep keeps sensors attached and irritation-free.
- Move regularly. Even a short walk after meals can lower glucose and reduce blood-pressure strain.
- Balance your plate. Combine carbohydrates with protein or fibre to slow absorption and protect vessel walls.
- Rest enough. Poor sleep pushes hormones that raise both glucose and blood pressure.
- Care for your skin. After removing a patch, follow gentle post-adhesive skin care to prevent redness or infection.

Patch tip
If your lifestyle involves heat, swimming, or heavy activity, reapply a fresh CGM patch every 10 days or sooner. Bundling your essentials through the Type Strong Product Bundle helps you stay stocked and saves on shipping.
People also ask
Can high glucose damage the heart without symptoms?
Yes. Blood-vessel and nerve damage often begins silently, which is why consistent monitoring and medical check-ups are vital.
What are the earliest signs of diabetes-related heart problems?
Many people first notice fatigue or shortness of breath, especially during exertion. Some feel mild chest tightness that comes and goes.
Does lowering blood sugar really reduce heart disease risk?
Absolutely. Studies by Diabetes UK and the American Diabetes Association confirm that good glucose control keeps arteries flexible and reduces future cardiovascular events.
Can a CGM help protect your heart?
A CGM can’t prevent heart disease directly, but by showing you trends, it lets you act early – adjusting meals, exercise, or medication before those spikes cause long-term strain.
A steady heart starts with steady monitoring
Managing your diabetes heart disease risk isn’t about perfection. It’s about knowing your patterns, protecting your skin, and using technology that keeps up with you. Each stable reading and secure patch adds to your overall confidence – not just in your numbers, but in your health.
At Type Strong, we believe in tools that help you stay consistent. Explore our full range of CGM patches, adhesive wipes, and bundle options to support reliable sensor wear and steady data – because caring for your heart starts with knowing what’s happening every day.
References
Diabetes UK. “Heart disease and diabetes.” Diabetes UK, 2024.
https://www.diabetes.org.uk/guide-to-diabetes/complications/heart
National Health Service (NHS). “Diabetes – complications.” NHS UK, updated 2024.
https://www.nhs.uk/conditions/diabetes/complications/
World Health Organization (WHO). “Cardiovascular diseases (CVDs).” WHO Fact Sheet, 2023.
https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Centers for Disease Control and Prevention (CDC). “Diabetes and Heart Disease.” National Center for Chronic Disease Prevention and Health Promotion, 2023.
https://www.cdc.gov/diabetes/library/features/diabetes-and-heart.html
American Diabetes Association (ADA). “Cardiovascular disease and diabetes.” Standards of Care in Diabetes – 2024.