Supporting a diabetic friend isn’t about grand gestures – it’s about understanding the daily demands of diabetes and offering steady, informed support. From navigating continuous glucose monitors (CGMs) to managing fatigue or low blood sugars, people with diabetes often carry a hidden burden. Your support can make a measurable difference in their mental and physical well-being.
The role of social support in diabetes management
Diabetes is a complex, chronic condition that requires constant self-management. According to Diabetes UK, support from friends and family plays a vital role in how well someone manages their diabetes. It can influence not only their emotional health but also their adherence to treatment plans and glucose control.
“When people with diabetes feel supported, they’re more likely to look after their health, stick to their treatment and cope better day-to-day.” – Diabetes UK
This support doesn’t have to be clinical. Simply understanding how their devices work, being mindful of food-related comments, or knowing how to respond to a hypoglycaemic episode are practical ways to be helpful.
Practical ways to support a diabetic friend
Here’s what support can look like in real life:
- Respect their management routine: People with diabetes often follow precise schedules for testing, medication, and meals. Disrupting these routines can affect glucose levels.
- Avoid judgmental questions: Phrases like “Can you eat that?” can be unhelpful and based on misconceptions. People with diabetes make decisions based on personal guidance from their medical team.
- Learn about their devices: Many people with diabetes use CGMs, insulin pumps, or infusion sets. Understanding what these do helps you offer practical support, especially in emergencies.
- Offer help during sensor changes: If your friend struggles with adhesive issues or skin sensitivity, they may appreciate assistance finding solutions, like better patch options or application tips.
- Listen when needed: Diabetes burnout is real. Providing a space to talk without offering unsolicited advice can be meaningful.
Understanding CGM patch challenges
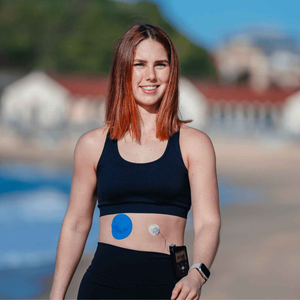
Many people with diabetes rely on CGMs like Dexcom or Libre to manage blood glucose in real time. These sensors often require adhesive patches to stay secure on the skin, especially during physical activity or hot weather.
Common patch-related concerns include:
- Adhesive not lasting the full sensor duration
- Peeling during workouts or hot days
- Skin irritation or redness

Supporting your friend could be as simple as recommending trusted options like:
- Dexcom G7 Patches – 20 Pack
- Dexcom G6 Adhesive Patches
- Freestyle Libre Adhesive Patches
- Medtronic Guardian & Infusion Set Patches
- Cut-to-Fit Tape Roll for custom coverage or overlapping areas
-
Build Your Own Patch Bundle for those using multiple devices
Each option is designed to provide a secure fit without compromising comfort – especially important for users with active lifestyles or sensitive skin. If your friend has concerns about adhesive ingredients, it’s best they consult a healthcare provider or dermatologist for specific guidance.
What not to say to someone with diabetes
Words matter. Some common phrases, while well-intentioned, may feel dismissive or misinformed.
|
Statement |
Why to avoid it |
|
“Are you allowed to eat that?” |
Implies restriction without understanding context |
|
“You don’t look diabetic” |
Minimises the invisible nature of the condition |
|
“Did you get diabetes from sugar?” |
Misinformation about the condition’s causes |
|
“I could never manage that” |
Centres your reaction instead of their experience |
|
“Just go low-carb” |
Offers advice that may not apply to their plan |
Universal ways to support
Support doesn’t need to be tailored only to close friends. In general settings – workplaces, schools, or community groups – the following practices help build a diabetes-friendly environment:
-
Provide access to hypo snacks like juice or glucose tabs if someone uses insulin
-
Make room in fridges for insulin or medications if needed
-
Allow flexibility for medical breaks
-
Avoid making assumptions about someone’s food choices or energy levels
-
Ask if they want assistance before acting
These actions are small, but they signal respect and awareness.
Help them stay active and confident
If your friend is sporty, travels frequently, or just leads a busy lifestyle, ensuring their CGM or infusion set stays put can be challenging. Encourage them to try medical-grade adhesive patches designed for movement, sweat, and extended wear.
You can suggest Dexcom G6 Patches or Libre Patches to reduce patch-related disruptions. These are waterproof, sweat-resistant, and come in different shapes for a tailored fit. They’re not a cure-all – but they often help with comfort, discretion, and sensor life.

For more information on how CGMs differ, see our in-depth Top 4 CGM Comparison for 2024 to better understand your friend’s tech.
Final thoughts: Consistency over perfection
Supporting a diabetic friend doesn’t require medical training or perfect knowledge. It simply involves being present, asking questions respectfully, and learning how to be useful when it matters most.
You might not know what to say every time. But when your friend sees that you care – whether through words, actions, or even something as small as picking up their go-to CGM patches – it shows.
https://typestrongworkspace.slack.com/archives/D08L34XJDRR/p1746846121593049
Explore Type Strong’s range of stay-put CGM patches to help your friend feel secure, supported, and ready to take on the day.