If you’ve ever woken up at 2am just to check a glucose reading, you know the feeling. The house is quiet, everyone’s asleep, but your mind is racing: what if the numbers have dropped too far? Many parents admit they half-sleep with one ear tuned for alarms. Adults with diabetes often say the same – setting multiple alerts on their phones, keeping glucose tablets or juice boxes by the bed, and never quite letting themselves drift fully into rest.
Continuous glucose monitors (CGMs) are a lifesaver in this routine, but alarms don’t always solve everything. Sometimes sensors peel off, sometimes alerts get missed. This is where implantable glucagon devices are being explored as a new kind of safety net – something that works in the background while you sleep.
Why night-time hypoglycaemia feels different
Low blood sugar during the day is disruptive, but at night it feels scarier. You might not notice the symptoms until they’re strong, or not at all. Parents often describe tip-toeing into their child’s room, just to double check. It’s not really about the numbers – it’s about the fear of missing one dangerous low in the dark.
This constant “what if” is why researchers pay so much attention to night-time lows. The American Diabetes Association has highlighted nocturnal hypoglycaemia as one of the biggest sources of stress for families. Even the best CGM patches and alerts can’t remove every worry.

What implantable glucagon devices actually do
Glucagon isn’t new – it’s the hormone that tells the liver to release stored glucose and raise blood sugar back into range. Traditionally it’s been delivered in an emergency by injection or, more recently, a nasal spray. The issue? It usually needs a caregiver to act fast, and mixing or preparing a kit in the middle of the night is stressful.
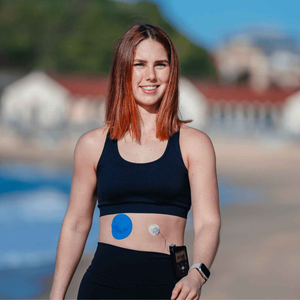
Implantable glucagon devices aim to take that step out of the equation. They sit under the skin and are designed to release glucagon automatically when levels fall too low. It’s not a replacement for your CGM, but more like a back-up parachute. Families already used to keeping sensors in place with CGM patches often describe the idea as reassuring: just as a patch stops a sensor from peeling off, glucagon could stop a sudden night-time drop from becoming something worse.
Comparing glucagon options for night-time safety
|
Option |
How it works |
When it is used |
Limitations |
|
Glucose tablets / gel |
Taken orally to raise sugar quickly |
First response to mild lows |
Needs waking, harder for kids at night |
|
Traditional glucagon kit |
Injection or nasal spray, emergency use |
Severe lows when unable to eat |
Needs prep, caregiver must act quickly |
|
Mini-dose glucagon pens |
Pre-measured, easier than mixing kits |
Moderate lows where eating isn’t possible |
Limited access, higher cost |
|
Insulin pumps with suspend |
Pauses basal insulin when CGM detects a low |
Prevents some overnight dips |
Relies on CGM accuracy, doesn’t raise sugar |
|
Implantable glucagon |
Auto-releases glucagon under the skin |
Severe or night-time lows |
Still under trial in most places |
People also ask
Can implantable glucagon stop night-time hypoglycaemia?
It won’t prevent every low, but studies suggest it can cut the risk of severe episodes by acting fast when glucose dips below a threshold. It works best as a backup alongside CGM monitoring.
Is implantable glucagon available for children?
Some trials have included children, but access depends on country approvals. Parents should check with their diabetes care team about availability.
Do I still need a CGM patch if I use glucagon?
Absolutely. A CGM gives you the trends and early warnings, while glucagon only steps in when sugar has already dropped. Reliable Dexcom G7 patches or Libre patches keep sensors secure at night, so alarms are less likely to be missed.
How is implantable glucagon different from a pump?
A pump with suspend mode stops insulin when a CGM predicts a low. Glucagon does the opposite – it actively raises blood sugar. For those already using infusion set patches, glucagon could one day become another layer of night-time protection.
The role of CGM patches in night safety
Here’s the thing: glucagon is backup. Your CGM remains the first line of defence. But if the patch lifts during the night, the alarm system fails. That’s why people swear by strong, breathable patches.
One dad told us he keeps a tape roll by the bed in case his son’s CGM starts peeling mid-sleep – a quick fix until morning. Another parent said swapping to longer-wear adhesive made the biggest difference, because she finally stopped hearing her child’s alarm going off for false detachment at 3am.
If you’ve faced similar issues, our guide to skin prep explains how to make patches last. And for children who scratch or tug at their sensors in bed, this post on kids and CGM patches shares parent-tested hacks. A patch bundle can also help families test which patch styles stay put through restless nights.
A hopeful future for families
Technology doesn’t erase the burden of diabetes, but it can ease it. For parents who’ve spent years setting alarms through the night, the idea of an implantable glucagon device isn’t just about science – it’s about finally sleeping through till morning. For adults living alone, it could mean knowing someone – or something – has their back if their sugars drop too far while they rest.

You don’t have to carry the worry alone. Between stronger CGM patches, adhesive support, and emerging safety tools like implantable glucagon, better nights are becoming possible. More sleep, less stress, and mornings that start with energy instead of exhaustion – that’s a future worth holding onto.
Disclaimer: This article is for educational purposes only and does not replace medical advice. Always consult your diabetes care team before making treatment decisions.
References
American Diabetes Association. (2023). Standards of Care in Diabetes. Diabetes Care, 46(Suppl. 1), S1–S290. Available at: https://diabetesjournals.org/care
Cryer, P.E. (2022). Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and Prevention. Endocrine Reviews, 43(2), 199–212.
Rickels, M.R., et al. (2021). Glucagon replacement in type 1 diabetes: Progress and challenges. The Lancet Diabetes & Endocrinology, 9(5), 326–336.
U.S. National Library of Medicine. (2023). Glucagon and diabetes research trials. ClinicalTrials.gov.