Insulin resistance is a condition that affects millions of people worldwide, often leading to serious health issues like Type 2 diabetes and heart disease. Despite its prevalence, many people are unaware of what insulin resistance actually is, how it develops, and the steps that can be taken to prevent or manage it. In this blog, we’ll explore the causes of insulin resistance, the symptoms to watch out for, and practical solutions to help manage or reverse the condition.
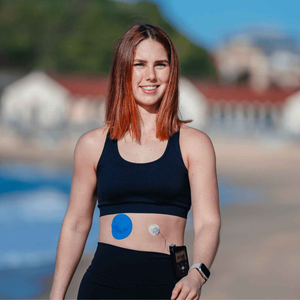
Before we continue, At Type Strong, we support individuals with diabetes by providing innovative products like our FreeStyle Libre, Medtronic Guardian & Dexcom G7 adhesive patches. Choose the best CGM for your needs and enhance your experience with our high-quality adhesive patches today!
Let's get started.
What is Insulin Resistance?
Insulin is a hormone produced by the pancreas that helps regulate blood sugar (glucose) levels by allowing cells to absorb glucose and use it for energy. Insulin resistance occurs when the body’s cells become less responsive to insulin, meaning that more insulin is required to help glucose enter the cells. As a result, blood sugar levels remain elevated, which forces the pancreas to produce even more insulin to compensate.
Over time, this increased demand for insulin can lead to higher blood sugar levels and the development of pre-diabetes or Type 2 diabetes. If left unmanaged, insulin resistance can also contribute to other serious health complications, including obesity, high blood pressure, and cardiovascular disease.
Causes of Insulin Resistance
Several factors can contribute to the development of insulin resistance. These include both genetic predispositions and lifestyle choices. Some of the most common causes are:
1. Excess Body Weight
Carrying excess weight, particularly around the abdomen, is one of the primary risk factors for developing insulin resistance. Fat cells, especially visceral fat (fat around the organs), produce inflammatory substances that can interfere with the body’s ability to use insulin effectively.
2. Physical Inactivity
A sedentary lifestyle increases the risk of insulin resistance. Regular physical activity helps improve insulin sensitivity by encouraging muscles to use glucose for energy. Inactivity, on the other hand, can cause glucose to accumulate in the bloodstream, leading to elevated insulin levels.
3. Poor Diet
Diets high in processed foods, added sugars, and unhealthy fats contribute to insulin resistance. Excessive consumption of refined carbohydrates, such as white bread, sugary snacks, and sugary beverages, can spike blood sugar levels and increase the body’s demand for insulin.
Learn about managing diet and blood sugar levels here.
4. Genetics
Family history and genetics also play a role in the development of insulin resistance. If you have a family history of Type 2 diabetes or metabolic syndrome, you may be more likely to develop insulin resistance.
5. Age
As people age, the risk of developing insulin resistance increases. Hormonal changes, reduced physical activity, and loss of muscle mass can all contribute to decreased insulin sensitivity over time.
6. Sleep Problems
Sleep disorders such as sleep apnea or chronic sleep deprivation are linked to insulin resistance. Inadequate sleep can disrupt the body’s hormone balance, leading to increased insulin production and reduced insulin sensitivity.
Symptoms of Insulin Resistance
Insulin resistance can develop gradually, and many people may not experience noticeable symptoms in the early stages. However, there are some signs and symptoms that may indicate the presence of insulin resistance:
1. Fatigue
Feeling tired or fatigued, especially after meals, can be a sign that your body is struggling to regulate blood sugar levels.
2. Increased Hunger
Insulin resistance can lead to higher insulin levels, which may cause frequent feelings of hunger, even after eating. This can result in overeating and weight gain.
3. Weight Gain
Unexplained weight gain, particularly around the abdomen, is a common symptom of insulin resistance. The body’s inability to properly use insulin can lead to fat storage, especially around the midsection.
4. Frequent Urination
Elevated blood sugar levels may cause the kidneys to work harder to eliminate excess glucose, leading to more frequent urination.
5. Dark Patches of Skin (Acanthosis Nigricans)
Darkened patches of skin, particularly in areas such as the neck, armpits, or groin, can be a visible sign of insulin resistance. This condition is known as acanthosis nigricans and is often associated with elevated insulin levels.
6. Difficulty Losing Weight
Individuals with insulin resistance may find it harder to lose weight despite efforts to diet and exercise. This is because insulin resistance can make the body store more fat.
Solutions for Managing and Reversing Insulin Resistance
The good news is that insulin resistance can be managed, and in some cases, even reversed with the right lifestyle changes. Here are some effective strategies to improve insulin sensitivity and reduce your risk of developing diabetes:
1. Adopt a Healthy Diet
Focus on a balanced diet rich in whole, unprocessed foods. Include plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats in your meals. Cut back on refined carbohydrates, sugary snacks, and sugary beverages, which can cause rapid spikes in blood sugar. Incorporate more fibre into your diet, as it helps slow down glucose absorption and stabilises blood sugar levels.
For CGM support, our FreeStyle Libre adhesive patches and Dexcom G7 patches provide peace of mind during dietary monitoring.
2. Increase Physical Activity
Regular physical activity is one of the most effective ways to improve insulin sensitivity. Aim for at least 150 minutes of moderate-intensity exercise, such as brisk walking or cycling, per week. Strength training exercises, such as weightlifting, can also help increase muscle mass and improve glucose uptake by the muscles.
For more information, here’s our guide to staying active and insulin sensitivity, offering insights and tips to help you incorporate movement into your daily routine.
3. Lose Weight
If you are overweight or obese, losing even a small amount of weight (5-10% of your body weight) can significantly improve insulin sensitivity. Focus on gradual, sustainable weight loss through healthy eating and regular physical activity.
4. Get Enough Sleep
Prioritise good sleep hygiene and aim for 7-9 hours of quality sleep per night. Address any underlying sleep disorders, such as sleep apnea, that may be contributing to insulin resistance.
5. Manage Stress
Chronic stress can elevate cortisol levels, which in turn can interfere with insulin’s ability to regulate blood sugar. Incorporating stress management techniques, such as meditation, deep breathing, yoga, or mindfulness, can help reduce insulin resistance.
6. Monitor Blood Sugar Levels
If you are at risk for or have already been diagnosed with insulin resistance, monitoring your blood sugar levels regularly is important. A Continuous Glucose Monitor (CGM), like the Dexcom G7 can help track your glucose levels in real-time, providing invaluable insights into how your body responds to different foods, activities, and stress.
7. Consult with a Healthcare Professional
Speak to your healthcare provider if you suspect you have insulin resistance. They can help assess your risk factors, order blood tests, and recommend personalised strategies to manage or reverse the condition.
Conclusion
Insulin resistance is a common but manageable condition that can lead to more serious health issues if left unchecked. By understanding the causes, recognising the symptoms, and implementing lifestyle changes, you can improve insulin sensitivity and lower your risk of developing Type 2 diabetes. Whether through adopting a healthier diet, staying active, or using tools like CGMs to monitor your blood sugar levels, managing insulin resistance is within your control.
Taking proactive steps now can help you lead a healthier, more balanced life in the future.
Sources:
1. Centers for Disease Control and Prevention (CDC). (2023). Insulin Resistance. Retrieved from https://www.cdc.gov/diabetes/about/insulin-resistance-type-2-diabetes.html
2. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2023). Insulin Resistance and Prediabetes. Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance#:~:text=Insulin%20resistance%20and%20prediabetes%20usually,appear%20in%20these%20same%20areas.
3. Mayo Clinic. (2023). What is insulin resistance? Retrieved from https://www.mayoclinic.org/diseases-conditions/obesity/multimedia/vid-20536756