Disclaimer: The information in this article is for educational purposes only. It is not a substitute for medical advice. Always seek guidance from your healthcare professional regarding your diabetes management.
When “doing everything right” still feels heavy
Some days, diabetes management can feel like a second full-time job. You count carbs, check glucose trends, correct a high, treat a low, and still wonder whether you’ve done enough. It’s not a lack of willpower — it’s mental fatigue.
People living with diabetes make hundreds of health-related decisions daily, from when to eat to how much insulin to administer. Research shows that this constant cognitive load contributes to diabetes distress and burnout, affecting both self-care and blood-glucose control (Kalra et al., 2018).

Psychologists define diabetes burnout as emotional exhaustion and detachment from diabetes tasks. It is common among long-term CGM users, particularly when technology adds noise instead of relief (Polonsky et al., 2020).
Why diabetes burnout happens (and why it’s not your fault)
Even with advanced tools, diabetes rarely lets you “switch off”. Sensors require calibrations, apps send alerts, and everyday stress compounds the strain. Over time, these layers of responsibility can lead to physical tiredness, emotional exhaustion, and frustration (Peyrot et al., 2019).
|
Common trigger |
What it looks like day-to-day |
Why it matters |
|
Constant alerts from devices |
Ignoring alarms or anxiety at every beep |
Creates “alarm fatigue” and missed readings |
|
Patch or sensor detachment |
Doubt in readings, frequent re-applications |
Increases cost and frustration |
|
Comparing results online |
Feeling inadequate or “behind” |
Reduces motivation |
|
Poor sleep or irregular routine |
Low mood, foggy concentration |
Worsens glycaemic variability |
Burnout is not failure — it is a human reaction to long-term medical pressure. Recognising it early helps prevent serious emotional decline (American Diabetes Association, 2023).
Turning technology from stressor into support
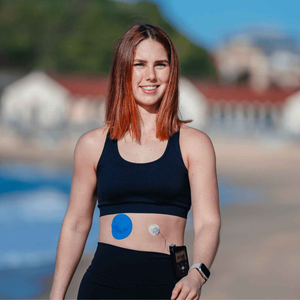
Digital diabetes tools, when aligned with your lifestyle, can lighten rather than add weight. Studies show that continuous glucose monitoring (CGM) improves glycaemic control and quality of life when users feel comfortable with their devices (Beck et al., 2017).
1. Secure your sensor for fewer interruptions
A dislodged sensor can trigger false alarms and stress. Using medical-grade CGM patches such as the Dexcom G7 patches or FreeStyle Libre adhesive patches maintains adhesion and reduces data gaps. Pairing with adhesive wipes supports consistent readings, particularly in heat or humidity.
2. Automate and schedule alerts
Adjust app notifications so only essential alarms interrupt your day. Research into “alarm fatigue” confirms that alert volume strongly affects stress and self-management behaviour (Tanenbaum et al., 2022).
3. Simplify your setup with bundles
Decision fatigue contributes to burnout. Keeping consistent patch types and prep tools in a bundle streamlines routines and avoids last-minute patch searches.

Further reading: Dexcom G7 users – why regular patches don’t always work.
Habits that lighten the mental load
Create deliberate downtime
Set “no-alert” windows when safe to do so. Regular rest lowers perceived diabetes distress (Kerr et al., 2021).
Pair care tasks with natural anchors
Link CGM checks with daily rituals — after brushing teeth or before meals. This repetition strengthens habit memory and reduces decision strain (Wood & Rünger, 2016).
Focus on proper skin prep
Good adhesion starts with clean, dry skin. Following proper skin prep techniques prevents irritation and keeps sensors stable, supporting long wear time and lower stress.
Adjust seasonally
Weather shifts influence patch performance and skin comfort. See why your CGM sensor needs extra protection in summer to prevent avoidable patch issues.
People also ask
What does diabetes burnout feel like?
Emotional exhaustion, detachment, irritability, and frustration with constant self-care. Some describe it as being “tired of doing everything right” (Polonsky et al., 2020).
Can technology make diabetes easier to manage?
Yes — consistent CGM use improves time-in-range and reduces stress when the user feels confident managing alerts (Beck et al., 2017).
Do better CGM patches prevent burnout?
They help indirectly by avoiding frequent re-applications and false sensor errors. Reliable adhesion contributes to trust in your device and less cognitive load.
When should I seek help?
If burnout affects sleep, relationships, or glucose stability, discuss it with your diabetes team. Psychological support tailored to chronic illness improves emotional resilience (Kalra et al., 2018).
The small resets that make a big difference
Burnout is not the end of control — it’s a reminder to rebuild balance. Whether through stronger CGM patches, supportive adhesive wipes, or an organised bundle set, every practical fix saves emotional energy.
Consistency and compassion go hand in hand. By using tech that supports your life, not dictates it, you can make diabetes management calmer, steadier, and more sustainable.
References
American Diabetes Association (2023) Standards of Care in Diabetes – 2023. Diabetes Care, 46(Suppl 1), S1–S316. Available at: https://diabetesjournals.org
Beck, R. W., Riddlesworth, T., Ruedy, K. J. et al. (2017) Effect of Continuous Glucose Monitoring on Glycemic Control in Adults With Type 1 Diabetes Using Insulin Injections: The DIAMOND Randomized Clinical Trial. JAMA, 317(4), 371–378.
Kalra, S., Kalra, B., Balhara, Y. P. S. (2018) Diabetes Distress and Diabetes Burnout: A Review of the Current Evidence. Diabetes Therapy, 9(4), 1933–1941.
Kerr, D., Barnard-Kelly, K., Matfin, G. (2021) Digital Resilience in Diabetes Care: Managing the Psychological Impact of Technology. Diabetes Spectrum, 34(3), 247–253.
Peyrot, M., Rubin, R. R., Lauritzen, T. et al. (2019) Psychosocial Problems and Barriers to Improved Diabetes Management: Results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN2) Study. Diabetic Medicine, 36(6), 716–727.
Polonsky, W. H., Fisher, L., Earles, J. et al. (2020) Assessing and Addressing Diabetes Burnout. Clinical Diabetes, 38(2), 116–124.
Tanenbaum, M. L., Hanes, S. J., Arakelyan, L. et al. (2022) The Human Side of Diabetes Technology: A Qualitative Study of Alarm Fatigue and Device Burden. Diabetes Technology & Therapeutics, 24(2), 96–104.
Wood, W. & Rünger, D. (2016) Psychology of Habit. Annual Review of Psychology, 67, 289–314.