Mastering Insulin Administration: 4 Ways to Manage Diabetes with Type Strong

For individuals with diabetes, managing blood sugar levels effectively often involves insulin therapy. Insulin is a hormone that helps regulate blood sugar levels by allowing glucose to enter cells, where it can be used for energy. However, administering insulin can be daunting for some. At Type Strong, we're committed to empowering individuals with diabetes to navigate their insulin therapy confidently. In this guide, we'll explore four common methods of insulin administration and provide practical tips for success.
1. Subcutaneous Insulin Injections
Injections are the most traditional method of insulin administration. This involves using a syringe or insulin pen to inject insulin into the fatty tissue just beneath the skin. Subcutaneous injections can be given in various areas of the body, including the abdomen, thighs, buttocks, and upper arms.
Tips for Insulin Injections:
- Rotate injection sites to prevent lipodystrophy (changes in fat tissue) and ensure consistent insulin absorption.
- Use proper injection technique, including holding the skin taut and inserting the needle at a 90-degree angle.
- Avoid injecting into scar tissue, bruises, or areas with active infections.
- Dispose of needles and syringes safely in a sharps container to prevent accidental needlestick injuries.
2. Insulin Pens
Insulin pens are convenient, prefilled devices that allow for precise insulin dosing and easy administration. Insulin pens come in disposable or reusable models and are available with different types of insulin (e.g., rapid-acting, short-acting, intermediate-acting, long-acting). Insulin pens typically use disposable needles that are screwed onto the pen device for each injection.
Tips for Insulin Pens:
- Familiarise yourself with the specific insulin pen model you're using, including how to prime the pen, dial the dose, and inject the insulin.
- Keep insulin pens stored properly according to the manufacturer's instructions, typically at room temperature once opened.
- Replace the needle before each injection to ensure sterility and prevent contamination.
- Be mindful of the expiration date of insulin cartridges or prefilled pens and discard them if expired.
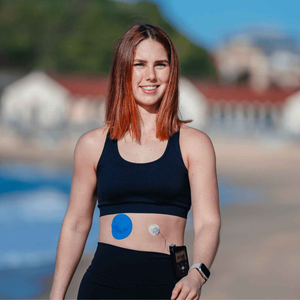
3. Insulin Pump Therapy
Insulin pump therapy, also known as continuous subcutaneous insulin infusion (CSII), involves wearing a small, battery-operated device that delivers insulin continuously throughout the day. Insulin pumps deliver rapid-acting insulin via a tiny catheter inserted beneath the skin, typically in the abdomen. Users can adjust basal (background) insulin rates and administer bolus doses for meals and corrections as needed.
Tips for Insulin Pump Therapy:
- Work closely with your healthcare provider or diabetes educator to set up and program your insulin pump according to your individual insulin needs and lifestyle.
- Monitor blood sugar levels regularly and adjust insulin pump settings as needed to maintain target blood sugar levels.
- Rotate infusion site locations regularly to prevent irritation or scarring.
- Keep spare infusion sets, reservoirs, and batteries on hand in case of pump malfunctions or emergencies.
4. Inhaled Insulin
Inhaled insulin offers an alternative to injectable insulin for some individuals with diabetes, particularly those who prefer to avoid injections or have difficulty with subcutaneous injections. Inhaled insulin is delivered via a handheld inhaler device that releases powdered insulin into the lungs, where it is absorbed into the bloodstream.
Tips for Inhaled Insulin:
- Follow the manufacturer's instructions for proper inhaler technique, including how to load the insulin cartridge, inhale the dose, and exhale slowly.
- Use inhaled insulin as directed, typically before meals, to cover mealtime insulin needs.
- Monitor blood sugar levels regularly and adjust insulin doses as needed based on your healthcare provider's recommendations.
- Be aware of potential side effects of inhaled insulin, such as coughing or throat irritation, and report any adverse reactions to your healthcare provider.
Conclusion: Taking Charge of Insulin Therapy with Type Strong
Managing diabetes with insulin therapy requires diligence, patience, and a willingness to learn. By exploring the various methods of insulin administration and implementing best practices for each, individuals with diabetes can take control of their insulin therapy and achieve optimal blood sugar management. At Type Strong, we're dedicated to providing the support, resources, and innovative products needed to empower individuals with diabetes on their journey to better health. Whether it's our adhesive patches for continuous glucose monitors or educational content like this blog, we're here to help you navigate your insulin therapy confidently and live your best life with diabetes.
Sources:
1. American Diabetes Association. (n.d.). Insulin Basics. https://www.diabetes.org/diabetes/medication-management/insulin-other-injectables/insulin-basics
2. Diabetes UK. (n.d.). Insulin. https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/insulin