In September 2025, NHS England confirmed that a laboratory equipment issue had caused inaccurate blood test results for thousands of people. The problem was traced to Trinity Biotech Premier Hb9210 HbA1c analysers, which were producing falsely high glucose readings. This led to as many as 55,000 people being misdiagnosed with type 2 diabetes or pre-diabetes (The Times).
The error was first identified at Luton and Dunstable Hospital, where about 11,000 patients were affected, but was later confirmed across 16 NHS hospital trusts (The Sun).
How many people were affected by the misdiagnosis?
The scale of the issue is significant. NHS estimates suggest that 55,000 patients may have received incorrect results between April 2024 and mid-2025 (Diabetes Research & Wellness Foundation).
Although the number sounds alarming, NHS England has emphasised that the clinical risk of harm is low. Fewer than 10 per cent of NHS laboratories were using the faulty equipment, and the majority of people tested during this period are unaffected (The Independent).
What happens if you were wrongly diagnosed with type 2 diabetes?
A diagnosis of type 2 diabetes often leads to major changes – medication, diet shifts, and lifestyle adjustments. If your results were inaccurate, you may have gone through unnecessary stress or treatment.
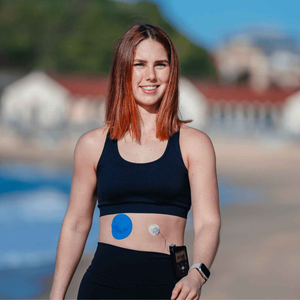
While the NHS believes the risk of long-term harm is minimal, the emotional weight of a misdiagnosis can’t be ignored. This is a reminder of why clear communication and accurate testing are so important. For CGM users, it also shows why many people choose to rely on technology to back up traditional testing. Having a continuous stream of data, supported by a secure CGM patch, can provide reassurance while bigger health systems work through these errors.

How is the NHS fixing the diabetes test error?
Once the issue was confirmed, the Medicines and Healthcare products Regulatory Agency (MHRA) issued safety guidance. All affected machines were recalibrated or removed, and new oversight procedures were put in place (DRWF).
The NHS is now contacting patients directly if their results need to be reviewed. Repeat blood tests are being arranged, and any unnecessary prescriptions are being assessed. This rapid action is intended to minimise both physical risk and the emotional stress of uncertainty.
What should you do if you are concerned about your test results?
If you think you might have been affected, here are some practical steps:
|
Step |
Why it matters |
|
Check your diagnosis date |
If you had an HbA1c test between April 2024 and now, your results may fall within the affected window. |
|
Wait to be contacted |
NHS trusts are proactively reaching out, so you don’t need to call immediately. |
|
Speak to your GP |
If you haven’t been contacted but are worried, ask your GP to review your case. |
|
Monitor your symptoms |
Be mindful of typical diabetes symptoms such as fatigue, thirst, and blurred vision. Report anything unusual. |
If you’re already using a CGM, this is where your device can give you daily reassurance. Just make sure you’ve done proper skin prep so your readings remain reliable and uninterrupted.
Why accurate diabetes testing matters for long-term health
Accurate testing underpins every decision about your health. Misdiagnosis can mean:
- Unnecessary medication that brings side effects.
- Lifestyle changes based on inaccurate results.
- Emotional stress for you and your family.
For those living with diabetes, this news highlights why tools like CGMs are so valued. When combined with durable adhesive wipes or an all-in-one product bundle, you can strengthen sensor wear time and reduce uncertainty, even if lab tests are under review.

You might also find it helpful to read about how long a CGM patch should last or what to do if your patch feels too weak for daily life.
People also asked
How do I know if my diabetes diagnosis is wrong?
If your diagnosis came between April 2024 and now, and you were tested in an NHS trust using the affected analyser, you may be contacted for a repeat test. If you’re unsure, ask your GP to review your results.
Can HbA1c tests be inaccurate?
Yes. While HbA1c is usually reliable, factors like anaemia, recent illness, or equipment calibration issues can affect accuracy. This is why some people use CGMs to cross-check trends over time.
What should I do if I was misdiagnosed with type 2 diabetes?
The NHS will contact affected patients, but you can also request retesting from your GP. If you’ve started medication, your doctor will review whether it should continue.
Will I need to keep testing if I use a CGM?
Yes. A CGM provides valuable daily insights, but it doesn’t replace laboratory blood tests for diagnosis. However, using a CGM with a secure CGM patch can help you spot unusual trends while waiting for formal retesting.
Staying informed without alarm
If you were recently diagnosed with type 2 diabetes, it’s understandable to feel unsettled by this news. But the NHS is taking active steps to correct errors, and the risk of harm is considered low.
The best thing you can do is stay informed, stay in touch with your GP, and use the tools at your disposal - whether that’s CGM data, hypoallergenic patches, or adhesive wipes – to feel more confident day to day.
You’re not alone in this. With accurate information and supportive resources, you can continue to manage your health with clarity, not fear.