Scientific research has progressed and improved the treatment options for Type 1 diabetes in leaps and bounds since the first life-saving discovery of insulin in 1921. Advancements in insulin development to enhance safety and effectiveness, and the emergence of new technologies in the glucose monitoring and insulin delivery field have assisted numerous people to better manage Type 1. Moreover, rigorous ongoing research efforts are currently being made to develop a cure in the hopes of either halting or reversing the autoimmune pathway that results in Type 1.
Many nonprofits and government organisations are collaborating and working towards preventing and ultimately finding a cure for Type 1. This article discusses some of the ongoing effort towards achieving these goals.
The Study of “Biomarkers”
The Juvenile Diabetes Research Foundation (JDRF) - the leading supporter of Type 1 research worldwide; and Benaroya Research Institute (BRI) - another world-renowned nonprofit research institute, are investigating the molecular mechanisms of the disease to better understand its progression and discover new methods of treatment. BRI and Dr. Martin J. Hessner from Max McGee Research Centre for Juvenile Diabetes are investigating “Biomarkers”, which are measurable and examinable components of blood and tissue samples to predict the risk and likelihood of the disease in individuals.
Beta Cells Regeneration
A prominent research front towards finding a cure for Type 1 is the Beta Cell Regeneration Programme supported by JDRF. This programme aims to find and establish the health and function of beta cells and develop therapies to generate new Beta cells.
As Type 1 diabetes is an autoimmune disease in which the body’s immune system attacks and destroys the insulin producing Beta cells in the pancreas. Swiss researchers have discovered that once the Beta cells are destroyed, certain cells in the pancreas can regenerate themselves into insulin producing cells. These cells are called Alpha cells and are responsible for secreting a hormone called glucagon that counteracts the effects of too much insulin and helps the body maintain normal blood sugar levels. After running numerous experiments on mice, these researchers found that when nearly all of the Beta cells were destroyed and insulin therapy was given, the Alpha cells instinctively transformed into functioning Beta cells. Furthermore, when an adequate amount of Alpha cells converted into Beta cells, insulin therapy was no longer needed.
The discovery holds immense potential. However, Andrew Rakeman the scientific programme manager of JDFR’s Beta Cell Regeneration Programme, suggested “cautious enthusiasm” for such findings. He further states that future research is needed to come to a guaranteed and lasting treatment. As the vulnerability of the Alpha cells (not normally attacked by the immune system) is required to be considered once they convert into Beta Cells.
Beta Cells Transplant & Stem Cells
Beta Cells Transplant and the use of Stem Cells to create indestructible insulin-producing pancreatic islets
Another avenue of promising research is targeted at replacing the Beta cells destroyed by the Immune system. Over the past decade, global efforts have been made to establish whether Beta cell transplants could in fact be the lasting cure for the disease. This process entails replacing damaged Beta cells with pancreatic islets containing healthy Beta cells from a donor. In 2020 the Westmead Institute for Medical Research stated that islet transplant is a short-term curative measure for Type 1 and recorded that over 100 of these transplants have been carried out in Australia.
However, it should be considered that this procedure still has challenges and drawbacks even though it is now funded by the Australian Government. The treatment is invasive and is only available for people with severely unstable Type 1. It also requires multiple transplants, a large number of cells from deceased human donors, lengthy waiting periods, and the lifelong dependency on immunosuppressant drugs to prevent the immune system from attacking the transplanted cells.
One suggested solution to some of these issues is the transformation or reprogramming of stem cells obtained from readily available human tissues into potentially unlimited numbers of islets suited for transplantation. Professor Shane Grey and his team of experts from the Garvan Institute of Medical Research are also developing islets that could be protected from immune attack to eliminate the need for immunosuppressant drugs. Experts also believe that there is a lot of potential in this field of research as manipulating islets is a lot less challenging than targeting the immune systems of patients.
Wrapping Up
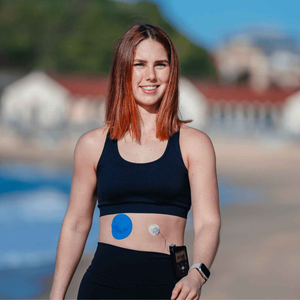
Embark on your journey with confidence and support. Complement the strides in Type 1 diabetes research. Our CGM patches stand as a simple yet powerful tool to enhance your daily management. Stay ahead in your health goals. Try our patches today and experience the ease they bring to your diabetes care. Your well-being matters, and we are here to make it a little bit simpler for you.
|
Our understanding of Type 1 diabetes and the available treatment technologies is advancing every day thanks to the efforts of these amazing organisations. We are definitely getting closer to a world without Type 1 diabetes - how exciting is that! If you'd like to read more on this topic, take a look at this post from JDRF regarding T1D Research Breakthroughs of 2020. |