If you live in the Asia-Pacific region, you might already notice how common type 2 diabetes has become. More people in workplaces, families, and schools are managing the condition — and often at younger ages than before. This isn’t just perception; lifestyle and healthcare pressures seem to be are driving a regional epidemic.
In this article, we explore why type 2 diabetes is rising so quickly, how lifestyle changes play a central role, and what this means for daily management.
The scale of type 2 diabetes in Asia-Pacific
Globally, around 537 million adults (aged 20–79) were living with diabetes in 2021, representing 10.5% of the global adult population (Sun et al. 2022). By 2045, this figure is projected to reach 783 million (12.2%). Asia is at the heart of this increase, with more than 60% of people with diabetes living in the region (Chan et al. 2009).
Current and projected figures
|
Country / Region |
Current estimate |
Projected by 2045 |
Key drivers |
|
China |
~148 million adults with diabetes (2024) (IDF 2024) |
~168 million (2050) (IDF 2024) |
Urbanisation, ageing, diet shifts |
|
India |
~77 million (2019) (Anjana et al. 2019) |
~134 million (2045) (Nanditha et al. 2021) |
Processed foods, sedentary work |
|
Indonesia |
11.3% adult prevalence (World Bank 2024) |
~16% (~40 million) (Rahmadhani et al. 2022) |
Limited healthcare access |
|
SE Asia region |
~10% prevalence baseline (IDF 2024) |
~13.2% (~185 million) (IDF 2024) |
Lifestyle and policy gaps |
|
Global |
537 million adults (2021) (Sun et al. 2022) |
783 million (2045) (Sun et al. 2022) |
+46% growth overall |
These figures show how type 2 diabetes trends Asia are rising beyond the global average, particularly in middle-income countries where prevalence is expected to increase by more than 20% between 2021 and 2045 (Magliano et al. 2021).

Why is type 2 diabetes increasing in Asia?
Several overlapping drivers explain why type 2 diabetes has become so prevalent in Asia-Pacific.
Urbanisation and sedentary lifestyles
Urban migration has shifted millions from agricultural or manual labour into office or service jobs. This change has reduced daily physical activity, with urban adults showing far higher diabetes prevalence than rural populations (Ramachandran et al. 2012).
Nutrition transition and processed foods
Diets in the region have moved from whole grains, legumes, and vegetables to refined carbohydrates, high-sugar snacks, and calorie-dense processed meals. The nutrition transition is now evident even in rural zones, increasing population-wide exposure to diabetes risk (Misra & Khurana 2011).
Genetic predisposition and the “Asian phenotype”
Many Asians are more likely to develop type 2 diabetes at lower BMI levels. This “Asian phenotype” is linked to greater visceral fat, reduced beta-cell function, and insulin resistance, even among those who appear lean (Yoon et al. 2006). Early life undernutrition and the so-called “thrifty phenotype” may further elevate lifetime risk (Hales & Barker 2001).
Healthcare access and awareness gaps
In many Asian countries, large numbers of people remain undiagnosed until complications appear. Weak primary care systems and stigma around diabetes limit early screening and timely lifestyle interventions (Chan et al. 2009).
Environmental and social pressures
Air pollution, chronic stress, and poor sleep are increasingly recognised as accelerators of insulin resistance. In India, long-term exposure to particulate matter (PM2.5) has been linked to increased diabetes incidence (Rajagopalan & Brook 2012).
What this means for daily life
For millions in Asia-Pacific, type 2 diabetes is no longer a late-life condition but a daily reality from younger ages. This means juggling family responsibilities, demanding jobs, and health management at the same time.

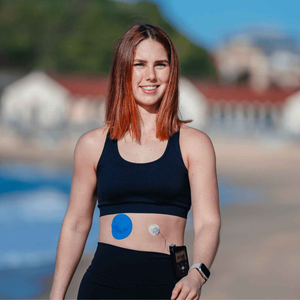
Continuous glucose monitors (CGMs) are increasingly part of the response, giving people real-time data on their blood glucose trends. To keep sensors secure in humid or active environments, many users rely on supportive CGM patches. These patches reduce sensor lift-off, particularly in hot climates or during physical activity.
Lifestyle adjustments are equally vital: short walking breaks during work hours, lowering sugary drink intake, and choosing fibre-rich local foods all play a role. You can also explore how athletes keep spare patches for confidence, or check how long a CGM patch should last to plan ahead for reliable wear.
People also ask
Why is type 2 diabetes increasing in Asia?
Urbanisation, sedentary jobs, processed food consumption, and genetic predisposition are driving faster increases compared with other regions (Yoon et al. 2006).
Which country in Asia has the highest diabetes rate?
China has the largest number of adults with diabetes (~148 million), while prevalence rates are also rapidly rising in India and Indonesia (IDF 2024).
How do lifestyle changes in Asia-Pacific affect diabetes risk?
Shifts away from traditional diets, reduced activity levels, and exposure to environmental risks such as stress and pollution are all increasing diabetes incidence (Misra & Khurana 2011).
Can CGMs help manage type 2 diabetes better?
Yes. CGMs provide continuous feedback on glucose levels, making it easier to adjust diet and medication. Using protective patches ensures sensors stay secure during daily life.
Living well despite rising trends
The statistics are daunting, but awareness is the first step. Fortunately, you can take steps in your own life: monitor glucose regularly, choose traditional whole foods, stay active, and use reliable tools like CGMs with patches for peace of mind.
You are not alone in this. With smarter healthcare systems, supportive products, and collective action, Asia-Pacific can shift from crisis to control. Every step — from a morning walk to a secure sensor patch — adds up to better management and stronger futures.
References
Anjana, RM, Deepa, M, Pradeepa, R, Mahanta, J, Narain, K, Das, HK, et al. (2019). Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR–INDIAB population-based cross-sectional study. The Lancet Diabetes & Endocrinology, 5(8), 585–596.
Chan, JCN, Zhang, Y, Ning, G. (2009). Diabetes in Asia and the Pacific: Implications for the global epidemic. Diabetes Care, 32(12), 227–229.
Hales, CN & Barker, DJP. (2001). The thrifty phenotype hypothesis. British Medical Bulletin, 60, 5–20.
IDF. (2024). IDF Diabetes Atlas. International Diabetes Federation. Available at: https://diabetesatlas.org
Magliano, DJ, Islam, RM, Barr, ELM, Gregg, EW, Pavkov, ME, Harding, JL, Tabesh, M, Koye, DN, Shaw, JE. (2021). Trends in incidence of total or type 2 diabetes: systematic review. BMJ, 372, n236.
Misra, A & Khurana, L. (2011). Obesity and the metabolic syndrome in developing countries. Journal of Clinical Endocrinology & Metabolism, 93(11 Suppl 1), S9–S30.
Nanditha, A, Ma, RCW, Ramachandran, A, Snehalatha, C, Chan, JCN, Chia, KS, Shaw, JE, Zimmet, PZ. (2021). Diabetes in Asia and the Pacific: implications for the global epidemic. Diabetologia, 59(3), 1–13.
Rajagopalan, S & Brook, RD. (2012). Air pollution and type 2 diabetes: mechanistic insights. Diabetes, 61(12), 3037–3045.
Ramachandran, A, Snehalatha, C, Shetty, AS, Nanditha, A. (2012). Trends in prevalence of diabetes in Asian countries. World Journal of Diabetes, 3(6), 110–117.
Sun, H, Saeedi, P, Karuranga, S, et al. (2022). IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates. Diabetes Research and Clinical Practice, 183, 109119.
World Bank. (2024). Diabetes prevalence (% of population ages 20–79). Available at: https://data.worldbank.org/indicator/SH.STA.DIAB.ZS
Yoon, KH, Lee, JH, Kim, JW, Cho, JH, Choi, YH, Ko, SH, et al. (2006). Epidemic obesity and type 2 diabetes in Asia. The Lancet, 368(9548), 1681–1688.